Trajectory of SARS COV2 virus: Why continued genomic surveillance is need of the hour
On the good side, Omicron’s arrival happened at a time when most populations were either vaccinated or had survived previous variants. This kept the death rates low.
By Newsmeter Network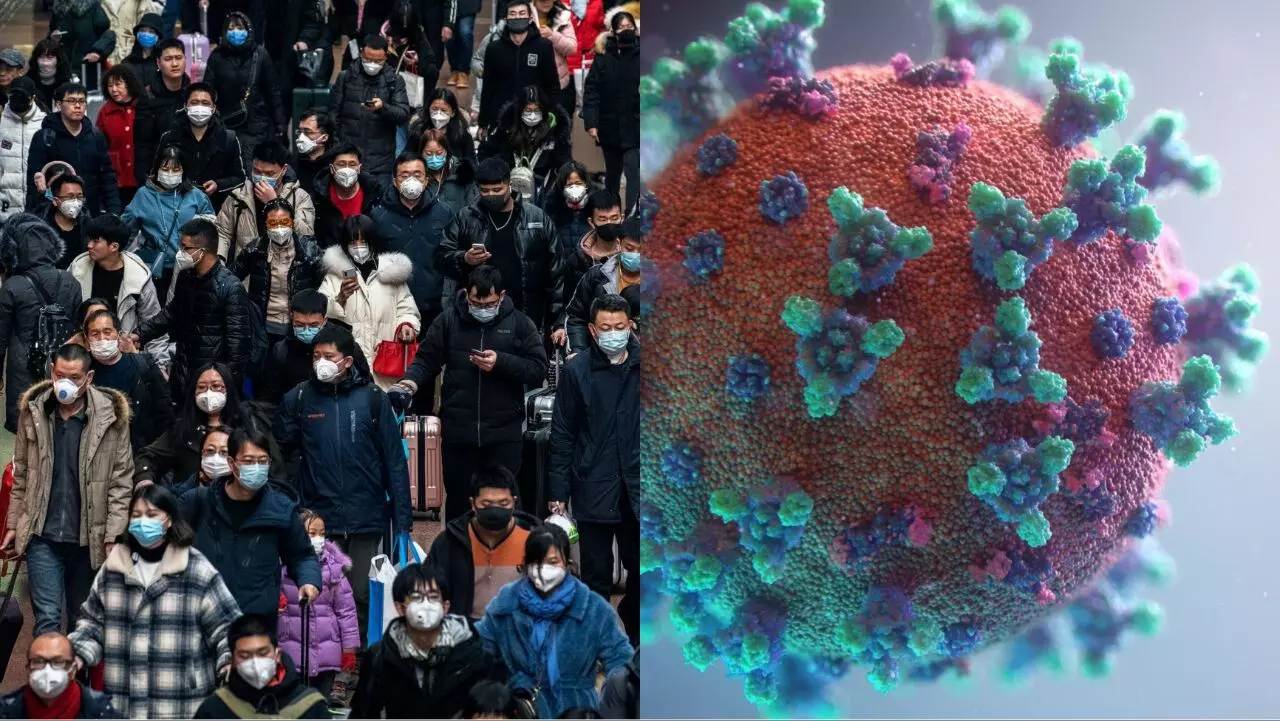
Hyderabad: The trajectory of the SARS-COV-2 virus over the past three years has been a subject of close monitoring and scientific interest across the world. A new pathogen unknown to mankind until then, the virus started its journey in China. Soon it arrived in Italy and then progressively involved multiple other nations, covering the globe in a matter of weeks.
The Original Strain
The original strain caused a significant amount of illness and death largely because of the lack of prior immune memory to this type of virus in the whole population. There was no protection offered by prior infection from other related coronaviruses either.
The mode of spread was initially believed to be through droplets, just like other common cold viruses. However, with the unfolding of multiple super spreader events, it became clear that this virus spread by aerosol, particularly in crowded, ill-ventilated indoor spaces where people would talk, laugh or sing. My article from 10 April 2020 was one of the first that outlined the exact mode of transmission of this virus (link). When the vocal cords rub against each other during the speech, an invisible vapor is created of weightless, tiny mucus particles laden with thousands of copies of the SARS CoV2 virus from an infected individual.
Because these mucus particles are weightless and small - only 5 to 10 µm in size, they would not settle with gravity and can circulate in closed spaces for several hours, with the ability to infect people who either share the same space at the same time or enter the area soon afterward.
There was an initial overemphasis on hand-washing and sanitization of hard surfaces such as table tops. This was due to a hangover from prior viral control measures prevailing until then.
A new disease and a new virus
COVID-19 was a new disease caused by a new virus and it took time for the world to realize the basics of its transmission. Unfortunately by then, extraordinarily large numbers of people had taken ill and also died. The disease had a propensity towards older age groups, whose mortality rates were multi-fold higher than that of younger adults. It caused little impact on children in terms of deaths, and apart from a rare complication called MIS-C, which was noted in the first two waves in particular, infection by this virus left the healthy pediatric population relatively unharmed.
Complications of Long Covid
Long Covid was another surprising complication, the initial signals of which came from 2020, (refer to my article, link). Unfortunately, the varied and often vague nature of symptoms, lack of confirmatory diagnostic laboratory tests, and nonavailability of specific treatment measures make this a condition that is difficult to cope with, not only for the patients but also their families as well as healthcare workers. Affected individuals continue to suffer greatly even following mild infections, particularly from the first wave. Search is ongoing for potential treatments.
Strategies of Countries
Different countries followed different strategies to control the pandemic,- especially in the first year. Some followed a zero Covid strategy, while others did the other extreme and that was the “let it rip” protocol. Both of these were severely criticized, and the “let it rip” strategy eventually translated into excess deaths of the order of tens of thousands.
Those countries that took early steps during the pandemic did relatively well. For instance, countries like India with large populations often living in crowded settings took early assertive measures during the first phase - where no treatments were available, mortality was at its highest, and the healthcare infrastructure had to be geared up to face an enemy unknown until then.
Once the healthcare workers and infrastructure were sufficiently prepared, the lockdown was relaxed and the disease gradually spread throughout the country.
Deaths continued to occur, but the discovery of dexamethasone as a treatment for pulmonary complications became one of the first true breakthroughs of 2020. When given at the right time for the right patient, steroids produced a survival benefit.
Fake Remedies
Meanwhile, opportunists cashed in by promoting all sorts of fake remedies, buoyed by the high spontaneous recovery rates that they cleverly claimed were the result of their intervention.
The arrival of vaccines was crucial in the fight against the pandemic because it was clear that the virus was causing harm among those who were immune naive that is those who had no prior immune memory of this virus.
While going through a natural infection also gives a chance of getting an immune memory, this is fraught with the risk of not only death but also long Covid and is therefore not a recommended strategy. That role was fulfilled by vaccines, whose complication rates were far lower than that of natural infection. Towards the end of 2020, vaccines were rolled out across the world. At this time, 98% of India’s population over the age of 12 has received at least one dose of vaccine, while 92% has received two doses.
Adaptability of the virus
Meanwhile, the virus showed its ability to rapidly adapt to the human immune response. With the arrival of variants one after the other, it became clear that this virus is here to stay for the long term. The most severe variant to attack a man so far was the Delta. Fast spreading and lethal, the delta caused carnage in almost every country, including India. The vaccination process was in its early stages when Delta hit the country. Many people lost their lives.
Advent of Omicron
Meanwhile, the virus continued to evolve and in November 2021, a landmark event occurred In South Africa with the discovery of a vastly different variant, thereafter named Omicron.
In just six weeks, Omicron covered the entire planet, causing a truly massive number of infections, the actual count of which will never be known.
Some estimates indicate that almost half the number of people living in a particular region was infected. On the good side, Omicron’s arrival happened at a time when most populations were either vaccinated or had survived previous variants. This kept the death rates low.
However, countries that followed the zero Covid strategy remained relatively immune naive, and therefore more vulnerable. In such countries, Omicron caused greater harm than in previously vaccinated and exposed countries.
Hong Kong is one such example, where mortality was extraordinarily high among unvaccinated seniors during the Omicron BA.2 wave in 2022. The virus continued to mutate - with multiple versions of Omicron ruling the world in early 2023 at the time of writing. The latest Omicron sub-lineage of concern is XBB 1.5 which is currently dominating the US and has extreme immune evasive properties. This means that it can infect people who had been previously vaccinated or infected or both.
Omicron in China
The rapid spread of COVID in China following the discontinuation of their dynamic zero COVID strategy is resulting in large-scale suffering and death. One-sixth of the planet’s population abruptly suffering an outbreak has made the entire world nervous. To date, no new variant has been reported as a result of this event or elsewhere, but it must be noted that there are large gaps in world genomic surveillance.
Low tide of Omicron in India
India is going through a prolonged “low tide” phase of the pandemic at this time, dominated by the XBB version of Omicron. Hospitals are not facing the burden of severe Covid cases like before, and no major wave has affected the country in the past 10 months. On the other hand, Japan had three waves in 2022 alone.
However, the situation could change with the arrival of either a grossly different version of Omicron or an entirely new variant - which could pop up in any corner of the world. Infections among people with compromised immune systems tend to be prolonged, allowing ample opportunity for the virus to pile on a series of mutations. The alpha variant, and possibly Omicron, are believed to have such an origin.
Continue genomic surveillance
Continued genomic surveillance is the need of the hour because this virus has the capability and opportunity to continuously evolve and change itself in ways that both evade the human immune response and also cause diseases of varying levels of severity.
There is no guarantee that the next variant will be milder than Omicron, but the fact that most of the world has achieved some form of hybrid immunity provides a certain level of security. The biological properties of the virus are determined by its genetic makeup - which is subject to change on a continuous and unpredictable basis. Therefore, a close watch is needed, while public health measures are followed to reduce the spread.
This virus rapidly spreads through the air. Masks help, particularly in closed, indoor gatherings. Improved room ventilation, social distancing, and restructuring of gatherings from indoors to outdoors are all layered measures that, when combined with vaccination, will reduce the overall impact of the pandemic.
Predictions, even by experts have repeatedly been wrong, and therefore long-term predictions are best avoided.
Article by (Dr. Rajeev Jayadevan - Medical doctor/specialist. Author, Educator, Co-Chairman of the National IMA COVID Task Force & Past President of the Indian Medical Association)