Judiciously use steroids: TS issues guidelines to combat 'black fungus'
Following a rise in Mucormycosis cases, commonly known as 'black fungus', in the state, the Telangana government on 15 May issued guidelines to prevent Mucormycosis during the second wave of the pandemic.
By Newsmeter Network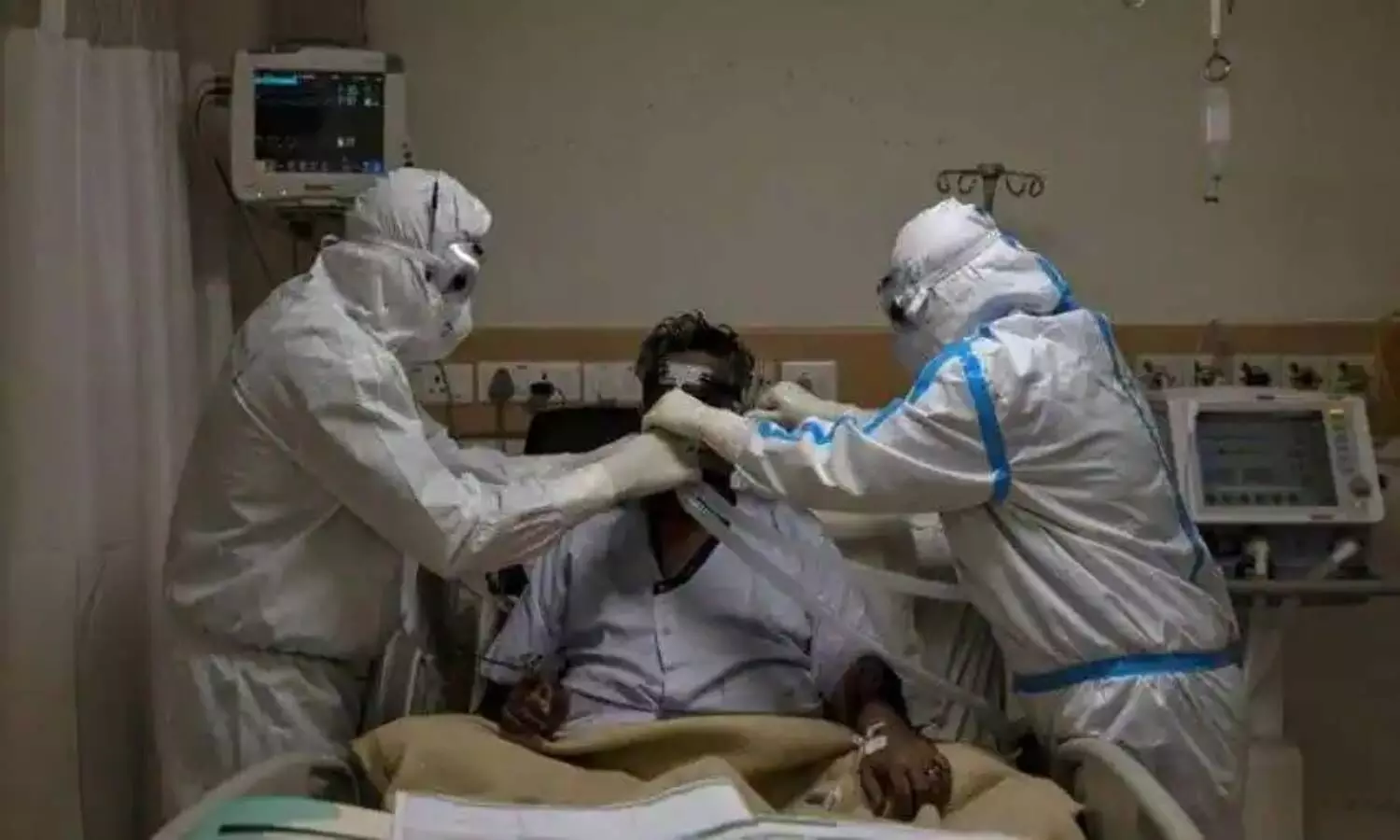
Hyderabad: Following a rise in Mucormycosis cases, commonly known as 'black fungus', in the state, the Telangana government on 15 May issued guidelines to prevent Mucormycosis during the second wave of the pandemic.
The government asked health specialist treating COVID-19 patients to use steroids judiciously and observe correct timing, dose, and duration. "Also use antibiotics/antifungals judiciously, and use clean, sterile water for humidifiers during oxygen therapy," said Dr. G. Srinivasa Rao, the director of public health, Telangana.
Incidences of Mucormycosis have been reported in COVID-19 patients from different parts of the country. A majority of these cases have been reported in patients who have recovered from the virus.
The government also prescribed SOPs to be strictly followed by all district medical and health officials, medical superintendents of all private hospitals, and practicing doctors.
Often Mucormycosis is caused due to poor maintenance of humidifiers. The government has asked patients to always use distilled or sterile water in humidifiers. "Never use unboiled tap water or mineral water. Fill up to about 10 mm below the maximum fill line. Do not let the water level pass below the minimum fill line," it said, adding that the water level should be checked twice daily and topped up as necessary.
The water in the humidifier should be changed daily and humidifiers should be washed in mild soap water, rinsed with clean water, and dried before reuse, it further said. It suggested soaking all components of the humidifier in mild antiseptic solution for 30 minutes then rinsing it with clean water and drying it once a week (for the same patient) and in between patients.
Why this sudden spike in Mucormycosis in COVID-19?
Black fungus or Mucormycosis can occur either concurrent to the COVID-19 infection or in the early post-recovery phase and affect the sinuses, eyes, and brain. Even though Mucor is present in the oral and respiratory lining of healthy individuals, it does not manifest as an infection in the presence of a healthy and intact immune system. Generally, this infection occurs in patients with uncontrolled diabetes, those undergoing cancer chemotherapy or on long-term steroid therapy, patients following organ transplantation and extensive burns and poly-trauma (severe injuries).
The COVID-19 virus causes a reduction in the lymphocyte (white blood cell) levels in the body. WBCs are the body's first line of defense against infections. Its failure allows for Mucor to attack the body and spread in the tissues. The current COVID management protocols require judicious but high dose steroid usage in those patients whose lungs have got affected. While helping to bring the COVID-related damage under control, the counter-effect of such high dose steroids is suppression of the body's immune mechanisms, which in turn makes our body more vulnerable to the adverse effects of this black fungus.
Certain drugs called immunomodulators used to treat severe cases of COVID-19 can cause immunosuppression. ICU admissions with long-term oxygen inhalation may result in a drop in oxygen mask hygiene. If the patient has pre-existing, poorly controlled diabetes, he/she is more at risk of developing Mucormycosis.
As the severity of the second wave is far more intense, more patients are being put on steroids and oxygen, and hence the increase in the cases of black fungus.